Ken Burns: HPV-Positive Base-of-Tongue Carcinoma Case Study
[fs-toc-h2]Overview
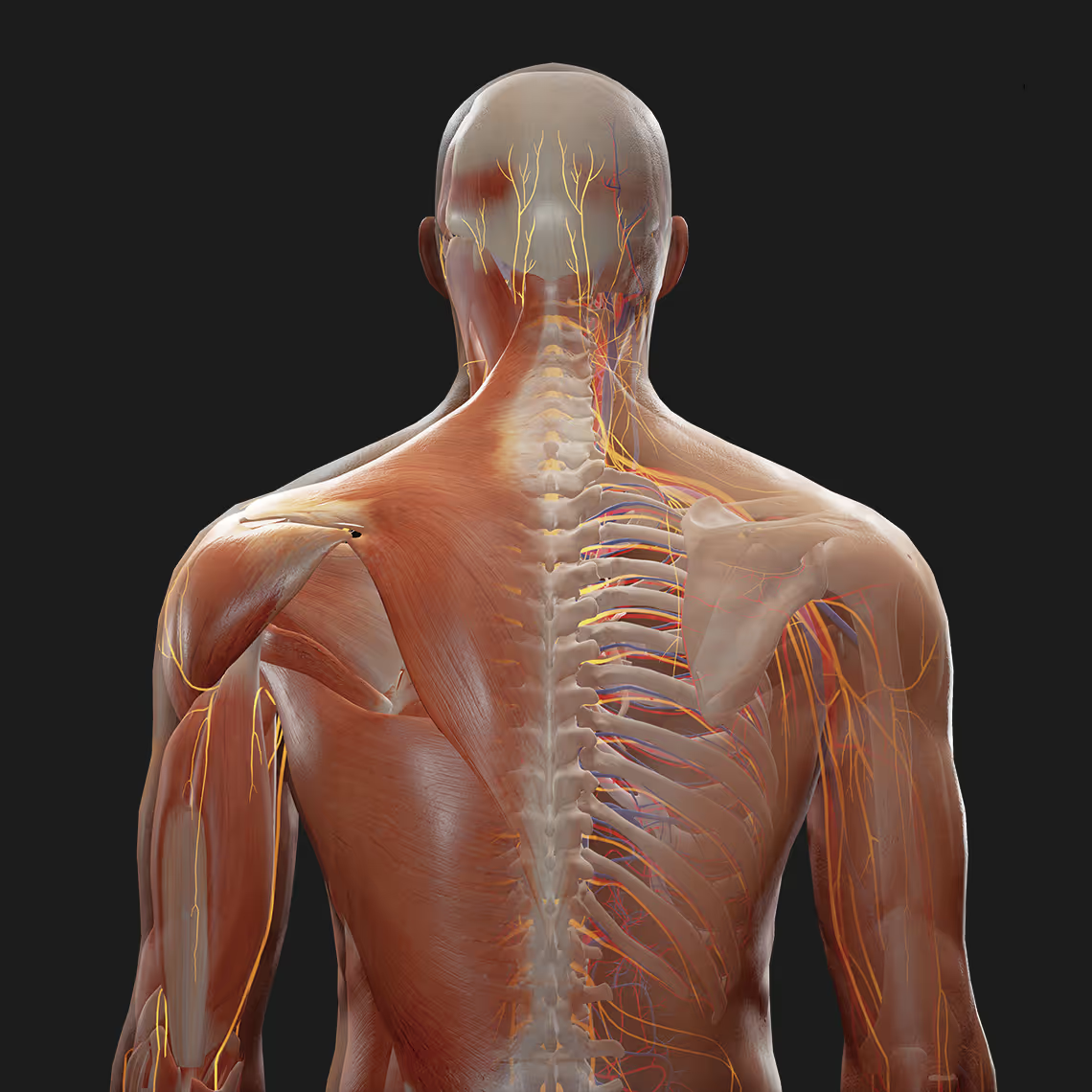
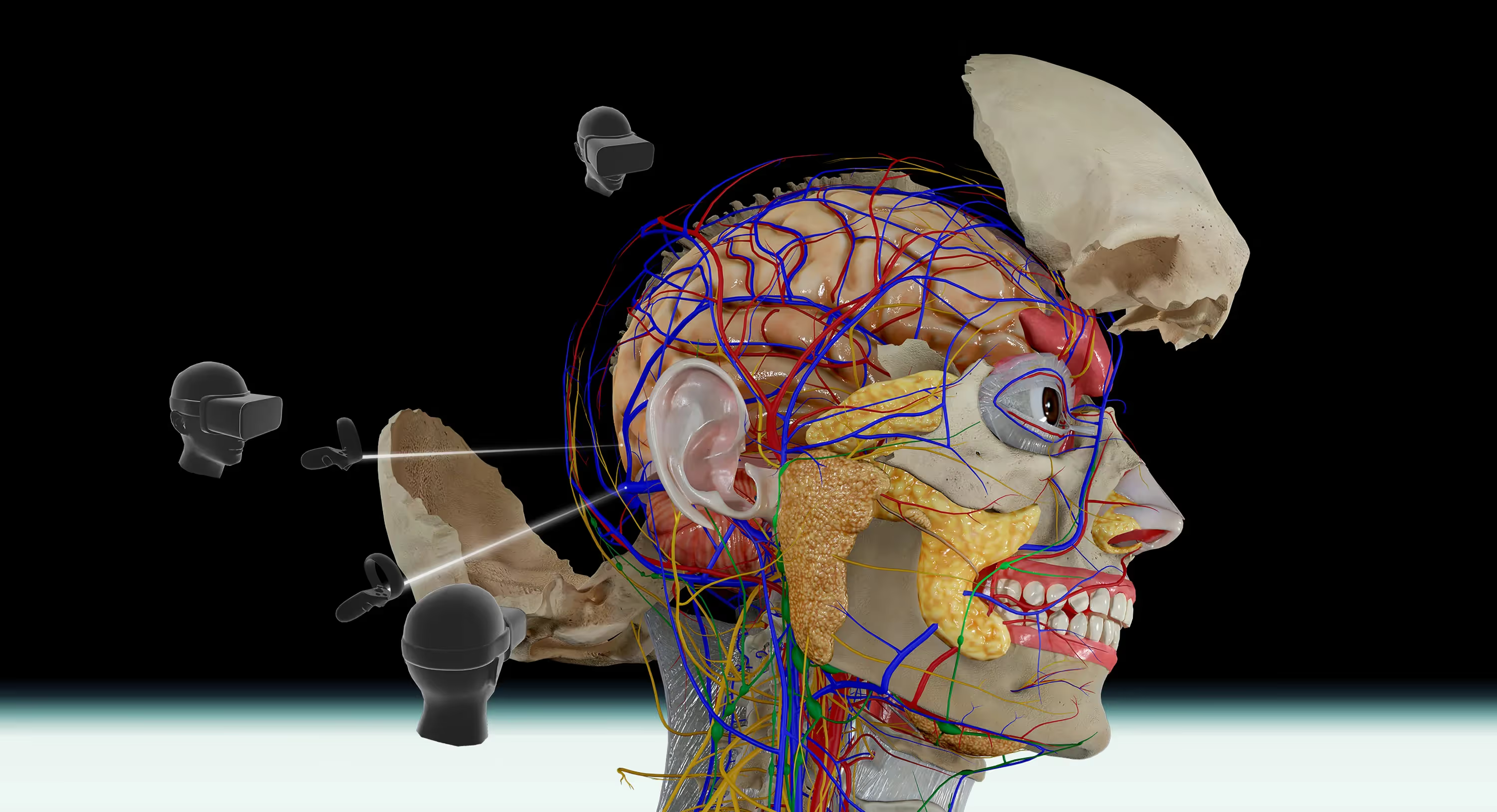
The following case study is inspired by patient data taken directly from the HNSCC Collection within The Cancer Imaging Archive (TCIA), a service that hosts an archive of publicly accessible de-identified cancer medical imagesThis content would need to be reframed to focus on how VR anatomy visualizatio...
Case Snapshot
[fs-toc-h2]Case Snapshot
Cancer: Head and neck
Type: Squamous cell carcinoma
Cancer site: Oropharynx
Diagnosis: Base-of-Tongue Carcinoma (BOT carcinoma)
[fs-toc-h2]Patient Introduction
Patient Introduction
Ken is a 50 year old Caucasian man who was shaving in the bathroom one day when he noticed a swollen lump on his neck. Not thinking much of it, he decided to ignore the enlarged mass and wait for it to subsideLike many patients, Ken initially dismissed the enlarged mass, hoping it would resolve on its own—a common response that highlights the importance of early medical evaluation for persistent symptoms. Two weeks later, the lump was still there.
[fs-toc-h2]Clinical Assessment
Clinical Assessment
After a visit to the doctor’s office, Ken’s primary care physician asked him a series of questions regarding his medical history and daily habits. A comprehensive patient history was taken, and questions inquiring into his daily activities and recreational habits were also asked to assess possible risk factors, including recreational drug use, sexual activity including number of recent sexual partners, smoking history and alcohol consumption.
With help from his doctor, Ken estimated that his smoking activity over the years amounted to ten pack-years, and indicated that he had quit a few years ago. Ken also admitted to havingKen reported multiple sexual partners over the years, though he wasn’t sure how that would help in determining his diagnosis—a key risk factor that students should recogniz. He had no family history of cancer, no history of recreational drug use and was not a fan of alcohol, drinking only during holidays and on special occasions..
Taking into account these findings, Ken’s primary care doctor ordered several tests and diagnostic images to be performed. A small sample of tissue was taken to check for signs of cancer and human papillomavirus (HPV). Computed tomography (CT) scans were also taken for a better picture of activity within the head and neck region.
Biopsy results showed a histology of squamous cell carcinoma from the tumor site with poorly differentiated cancer cells, and the pathology report on Ken’s HPV status came back as positive. Based on information about Ken’s updated patient history and risk factors, as well as results from diagnostic tests and imaging, ultimately a diagnosis was made for base of tongue carcinomaBased on Ken's risk factors, his physician ordered targeted diagnostic tests: . The physician carefully assessed all findings and Ken’s cancer was staged as IVB with TNM of 1, 3, 0. This clinical stage at presentation is consistent with studies which have shown that HPV-positive oropharyngeal squamous cell carcinoma tumors more likely present with early T stage (i.e., T1-T2), advanced N stage (i.e., usually cystic and multi-level), and have distinct histological features showing moderate or poor tumor differentiation.1
The biopsy revealed two critical findings that students should note: squamous ...
Pack-year:
TNM:
[fs-toc-h2]Head & Neck Cancer
Head & Neck Cancer
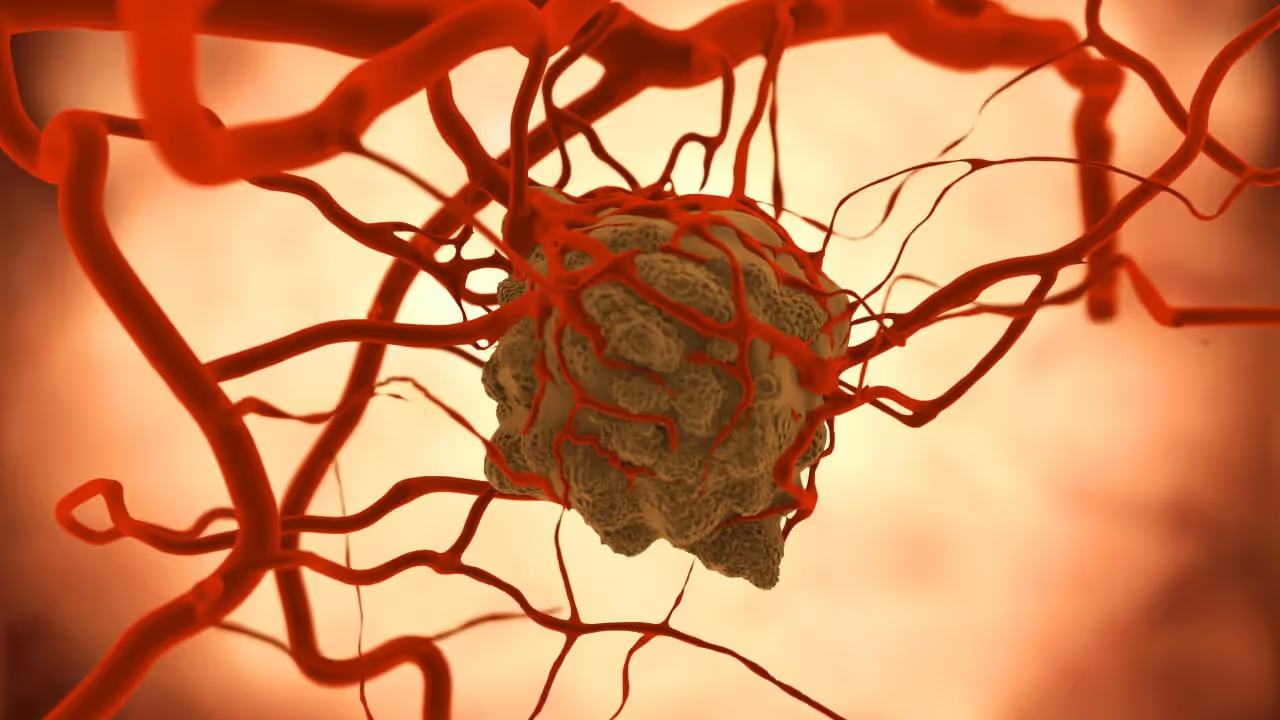
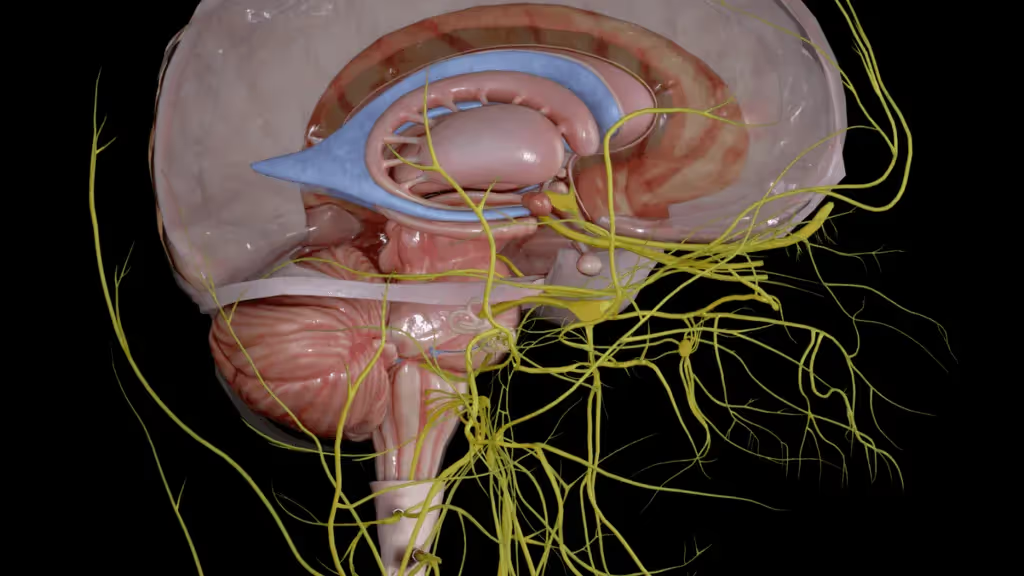
Head and neck cancer is a collective group of cancers that starts in the mouth, nose, throat, larynx, sinus, or salivary gland. These cancers account for approximately 4% of all cancers in the United States2 and about 95% of these are squamous cell carcinomas. Cancers of the head and neck can be categorized by the site in which the cancer begins: oral cavity, oropharynx, nasopharynx, hypopharynx, glottis (larynx), or sinus. In the case of Ken, the tumor is located at the base of the tongue, which is part of the oropharynx...
Head and neck cancers are more thanRecent SEER data (2024) indicate that head and neck cancers remain over twice as common among men as they are among women3 and diagnosed more often among people over 50 years of agecompared to women,3 and are most frequently diagnosed in individuals over the age of 50. Tobacco use, heavy alcohol use, and HPV infection increase the risk of head and neck cancersMajor risk factors include tobacco use, heavy alcohol consumption, and infection with human papillomavirus (HPV).
[fs-toc-h2]Base of Tongue Carcinoma
Base of Tongue Carcinoma
Base of tongue carcinoma-of-Tongue Carcinoma (BOT carcinoma) is a type of head and neck cancer that develops in the back third of the tongue. Most base of tongue cancersBase-of-Tongue Carcinoma (BOT carcinoma) cases are squamous cell carcinomas which form in the thin and flat cells that line the larynx, thyroid, throat, nose, and mouth. The area of the base of tongue is part of the oropharynx, which includes the tonsils, walls of the throat, and soft palate4[Learn more about base of tongue cancer (UT Southwestern, opens in new tab)](https://utswmed.org/conditions-treatments/base-tongue-cancer/).
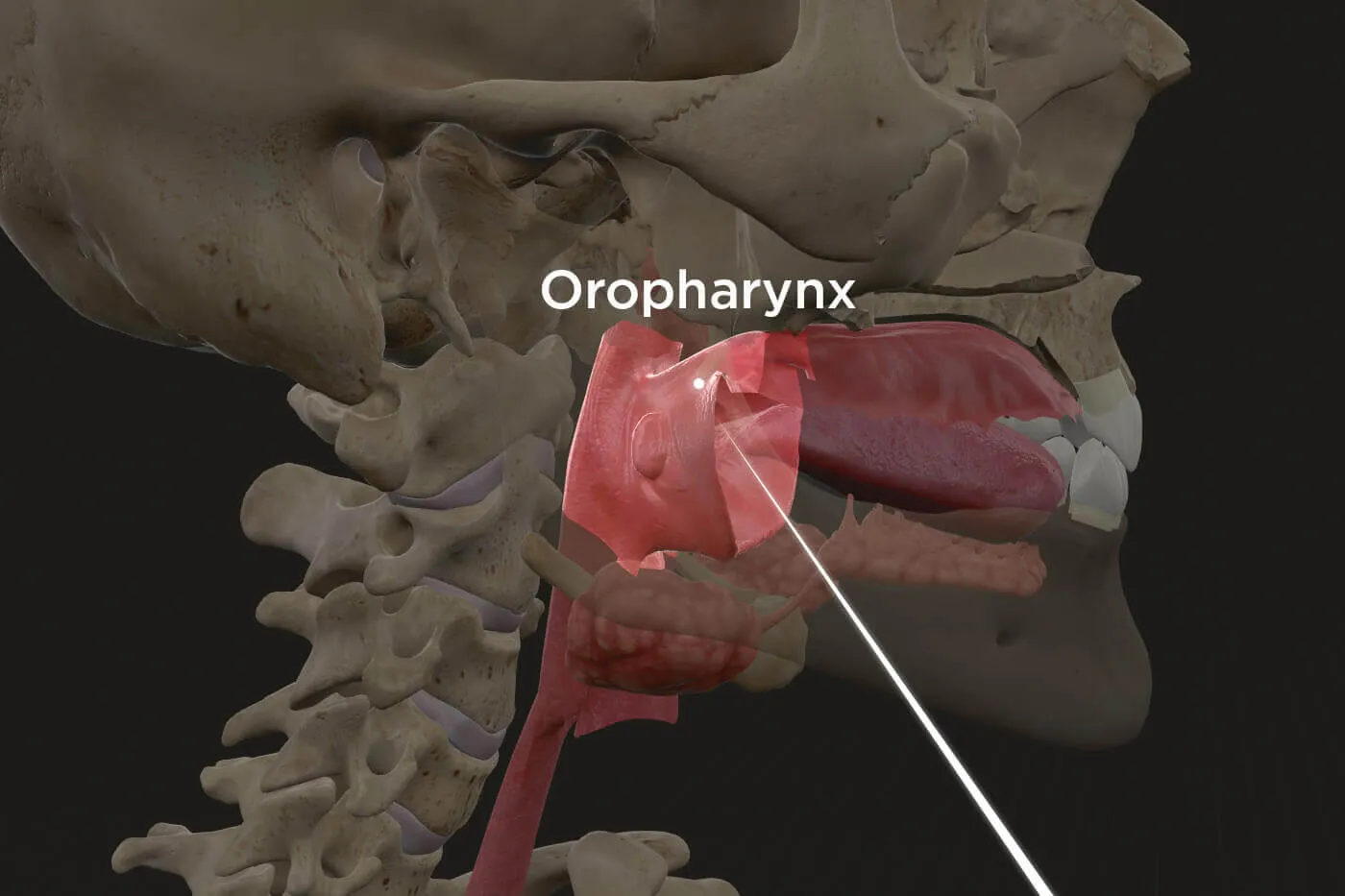
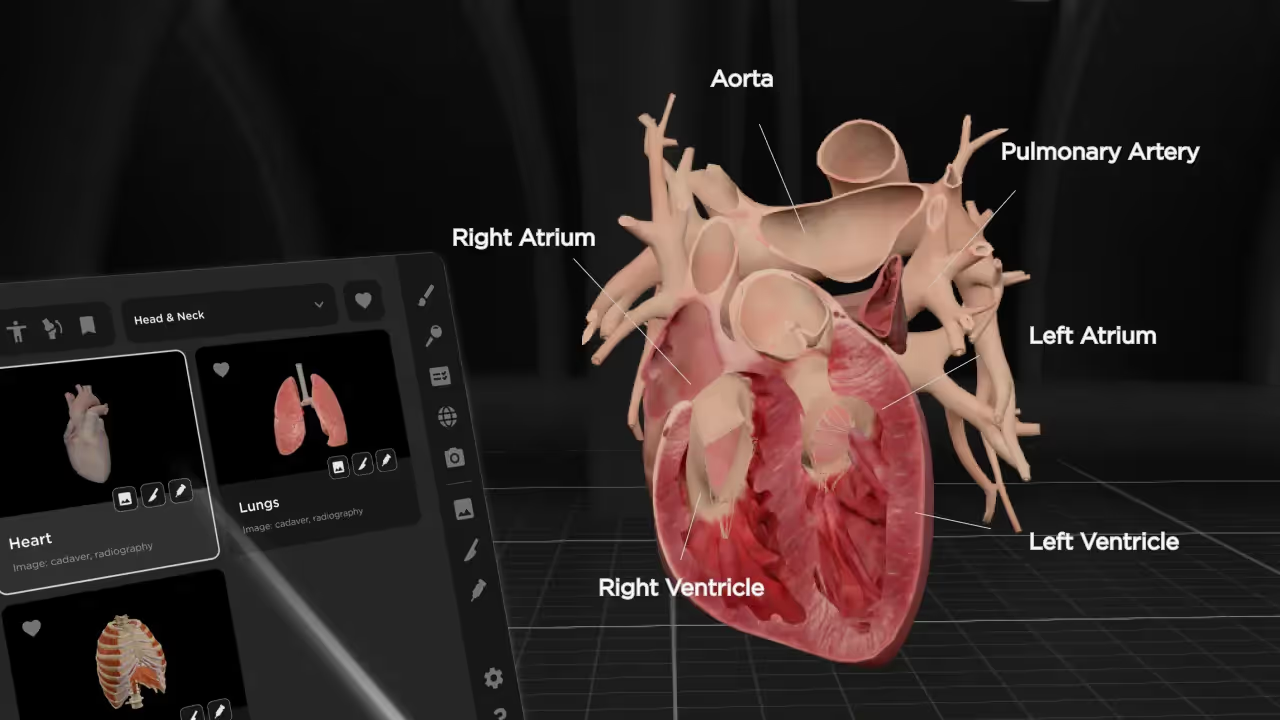
The image of the oropharynx is taken from the Bodymap VR application.
Ken, being male, middle-aged, Caucasian, HPV-positive, having a moderately high level of sexual activity with multiple partners, with histology of poorly-differentiated squamous cell carcinoma, fits the profile of a patient having characteristics consistent with HPV-positive oropharyngeal cancer:acti...
HPV is detectable in ~80% of oropharyngeal cancers [Smith et al., 2023].
Multiple sexual partners: sexual activity involving early first sexual relations, multiple partners, or oral sex, is characteristic of HPV-positive patients who have head and neck cancer located at the base of the tongue[HPV in Head and Neck Cancer Presentation (SlideShare, opens in new tab)](https://www.slideshare.net/priyankshah965/latest-presentation-of-hpv-in-head-and-neck); also, sexual behaviors are typically associated with HPV-positive head and neck squamous cell carcinomas but not with HPV-negative head and neck squamous cell carcinomas, which are mostly caused by tobacco and alcohol use [Behavioral risk factors for HPV-positive vs. HPV-negative head and neck cancers (NCBI, opens in new tab)](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4385715/)
[fs-toc-h2]Treatment Planning
Treatment Planning
After an extensive discussion on possible treatment options, Ken’s healthcare team decided to proceed with an oncologic treatment plan involving concurrent chemoradiotherapy treatment without induction chemotherapy or surgery.
[fs-toc-h2]Radiotherapy
Radiotherapy
Prior to the actual start date of initiating radiation treatment, the radiation oncologist arranged for Ken to go through a simulation process that involved placing Ken on a simulation machine, measuring his body and marking parts of immobilization devices to make sure that during actual radiotherapy, radiation beams would be delivered safely and precisely to the intended locations11.
Making the appropriate preparations and mapping out exact locations of where the treatment beams would be delivered is an important step prior to proceeding with actual radiotherapy treatmentThis simulation process is crucial for treatment success—it ensures radiation beams target the tumor precisely while protecting healthy tissue, a concept that's fundamental to understanding modern radiotherapy.
During simulation, a CT scan was used to capture images of Ken’s tumor and normal tissue from various angles, and specifically at areas to be treated with radiation. The radiation therapist carefully guided Ken through the simulation process to create a treatment position that was accurate, reproducible, and specific to Ken’s requirements by using a combination of immobilization devices including masks, leg molds, headrests, sponges, and pillows.12[Proton Therapy Preparation and Simulation (Seattle Cancer Care Alliance, opens in new tab)](https://www.seattlecca.org/treatments/proton-therapy/getting-treatment)
This CT simulation process which typically takes place approximately one week prior to the first actual radiotherapy session is important for Ken’s healthcare team to be able to properly perform accurate treatment planning and calculate the exact dose of protons to be precisely delivered to the target tumor.13[CT Simulation for Radiation Oncology (Emory University, opens in new tab)](https://radiationoncology.emory.edu/patients/treatments/ct_simulation.html)
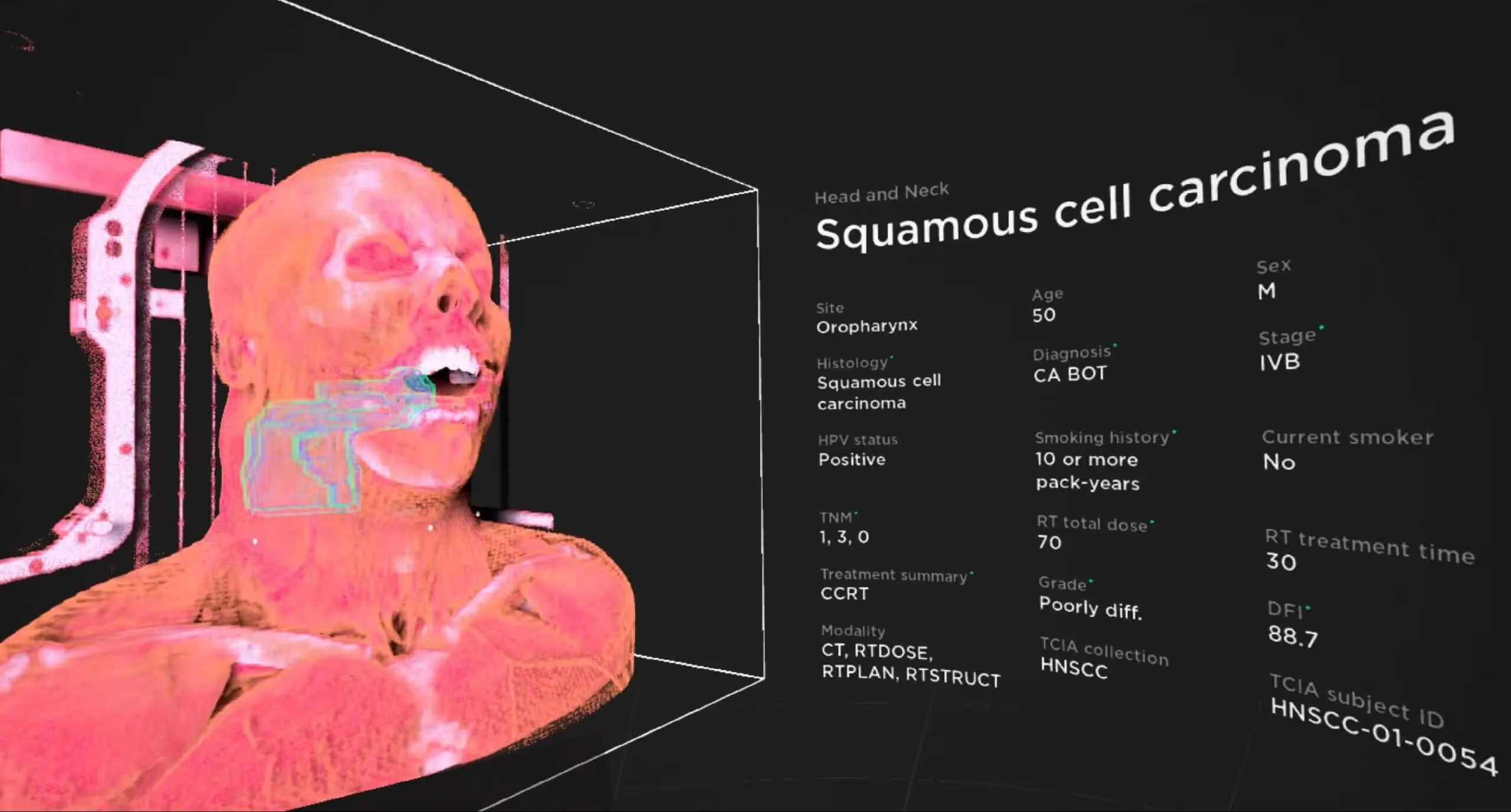
The image above is taken from the Cancer Library VR, and contains image and clinical data obtained from The Cancer Imaging Archive (TCIA), HNSCC Collection19[TCIA HNSCC Collection Overview (opens in new tab)](https://wiki.cancerimagingarchive.net/pages/viewpage.action?pageId=24281354) (TCIA subject ID: HNSCC-01-0054), with anonymized patient data and de-identified radiotherapy simulation scan showing physician- and dosimetrist-contoured target and avoidance volumes.
[fs-toc-h2]Chemotherapy
Chemotherapy
For the chemotherapy portion of the concurrent chemoradiotherapy treatment, Ken’s physician considered various chemotherapy agents and prescribed carboplatin, an agent best indicated for Ken and commonly used concurrently with radiotherapy.
[fs-toc-h2]Treatment summary
[fs-toc-h2]Treatment Summary
Ultimately, Ken’s treatment plan involved weekly administration of the chemotherapy agent carboplatin at a dose of AUC 2.0, given concurrently with a radiation dose of 70 Gy in 35 fractions to the tumor, taking place over a treatment period of 30 days.
[fs-toc-h2]Follow-up
Follow-up
By following his healthcare team’s carefully crafted concurrent chemotherapy treatment plan, Ken successfully achieved complete response. At the most recent follow-up appointment between Ken and his primary care physician, taking place just over 7 years after completing radiotherapy treatment, Ken was assessed's doctors assessed him to be alive and healthy without cancer recurrence, with a disease-free interval of over 88 months.
Ken’s healthcare team, and particularly the team in charge of Ken’s radiation treatment portion, were not all that surprised to learn about this happy outcome, as studies have shown that HPV-related oropharyngeal squamous cell carcinoma is extremely sensitive to radiation exposure and those indicated for treatment tend to be complete responders and long-term survivors's positive response aligns with clinical expectations for HPV-positive oropharyngeal cancers, which typically show excellent treatment response—an important prognostic factor for students to understand.14
This positive outcome is also consistent with studies showing that, in general, treatment outcome is much better and more curable when the cancer in question is HPV-related rather than tobacco- and alcohol-related15[Treatment outcomes by cancer etiology (Medical Dosimetry, opens in new tab)](https://www.medicaldosimetry.org/default/assets/File/denver2018/Zurek_Head_and_Neck_Cancer_in_The_Emerging_Era.pdf).
In fact, throughout the visits to the doctor’s office and discussions on treatment plans, Ken often had concerns that he would not beat this cancer, or even if the cancer were treated that it would return at a later datePatient anxiety about treatment outcomes is common in these cases, making it important for healthcare providers to understand the significantly better prognosis associated with HPV-positive tumors. He found himself increasingly regretful about certain liberties he took in his personal life, such as thoughts that he should have toned down his sex life involving multiple partners.
However, Ken’s physician offered reassurance through several research studies demonstrating that being HPV-positive in his case was not actually worse than being HPV-negative. In actuality, patients with HPV-positive base of tongue cancerBase-of-Tongue Carcinoma (BOT carcinoma) had a significantly better overall and disease-free survival compared to those with HPV-negative tumors16[HPV-positive base of tongue cancer outcomes (Wiley, opens in new tab)](https://onlinelibrary.wiley.com/doi/pdf/10.1002/ijc.25625). HPV-positive oropharyngeal cancer patients have 28-80% reductions in risk of death compared to HPV-negative patients, and are relatively much more likely to have improved outcomes17[Risk reductions in HPV-positive oropharyngeal cancer (PubMed, opens in new tab)](https://pubmed.ncbi.nlm.nih.gov/22782220/).
Ken now lives with his two dogs and has, since finishing treatment, largely abstained from some of his previous hobbies and used the extra time to pursue new interests such as swimming and cycling's successful treatment outcome demonstrates the excellent prognosis for HPV-positive oropharyngeal cancers when treated with appropriate concurrent chemoradiotherapy protocols. His advice to anyone facing a similar situation is to properly research and find an experienced physician and specialist team including radiation oncologists and radiation therapists who will be able to form an effective treatment plan and deliver the best possible care.
[fs-toc-h2]Reference
Reference
Special acknowledgement to the researchers and institutions that provided the Soft-tissue-Sarcoma collection datasets on TCIA:
Conclusion
This case study highlights the importance of early detection, risk factor ass...
Data Citation:
Grossberg A, Mohamed A, Elhalawani H, Bennett W, Smith K, Nolan T, Chamchod S, Kantor M, Browne T, Hutcheson K, Gunn G, Garden A, Frank S, Rosenthal D, Freymann J, Fuller C.(2017). Data from Head and Neck Cancer CT Atlas. The Cancer Imaging Archive. DOI: 10.7937/K9/TCIA.2017.umz8dv6s
Publication Citation:
Grossberg A, Mohamed A, Elhalawani H, Bennett W, Smith K, Nolan T, Williams B, Chamchod S, Heukelom J, Kantor M, Browne T, Hutcheson K, Gunn G, Garden A, Morrison W, Frank S, Rosenthal D, Freymann J, Fuller C. (2018) Imaging and Clinical Data Archive for Head and Neck Squamous Cell Carcinoma Patients Treated with Radiotherapy. Scientific Data 5:180173 (2018) DOI: 10.1038/sdata.2018.173
Clark K, Vendt B, Smith K, Freymann J, Kirby J, Koppel P, Moore S, Phillips S, Maffitt D, Pringle M, Tarbox L, Prior F. (2013) The Cancer Imaging Archive (TCIA): Maintaining and Operating a Public Information Repository, Journal of Digital Imaging, 26:6 pp 1045-1057. DOI: 10.1007/s10278-013-9622-7
Begin your VR anatomy journey today, sign up for a 7-day free trial.
Surgical & Clinical Specialties
Learn how to navigate the 3D model and utilize the tools to master human anatomy—all in one place.




.avif)


.avif)
.avif)